-
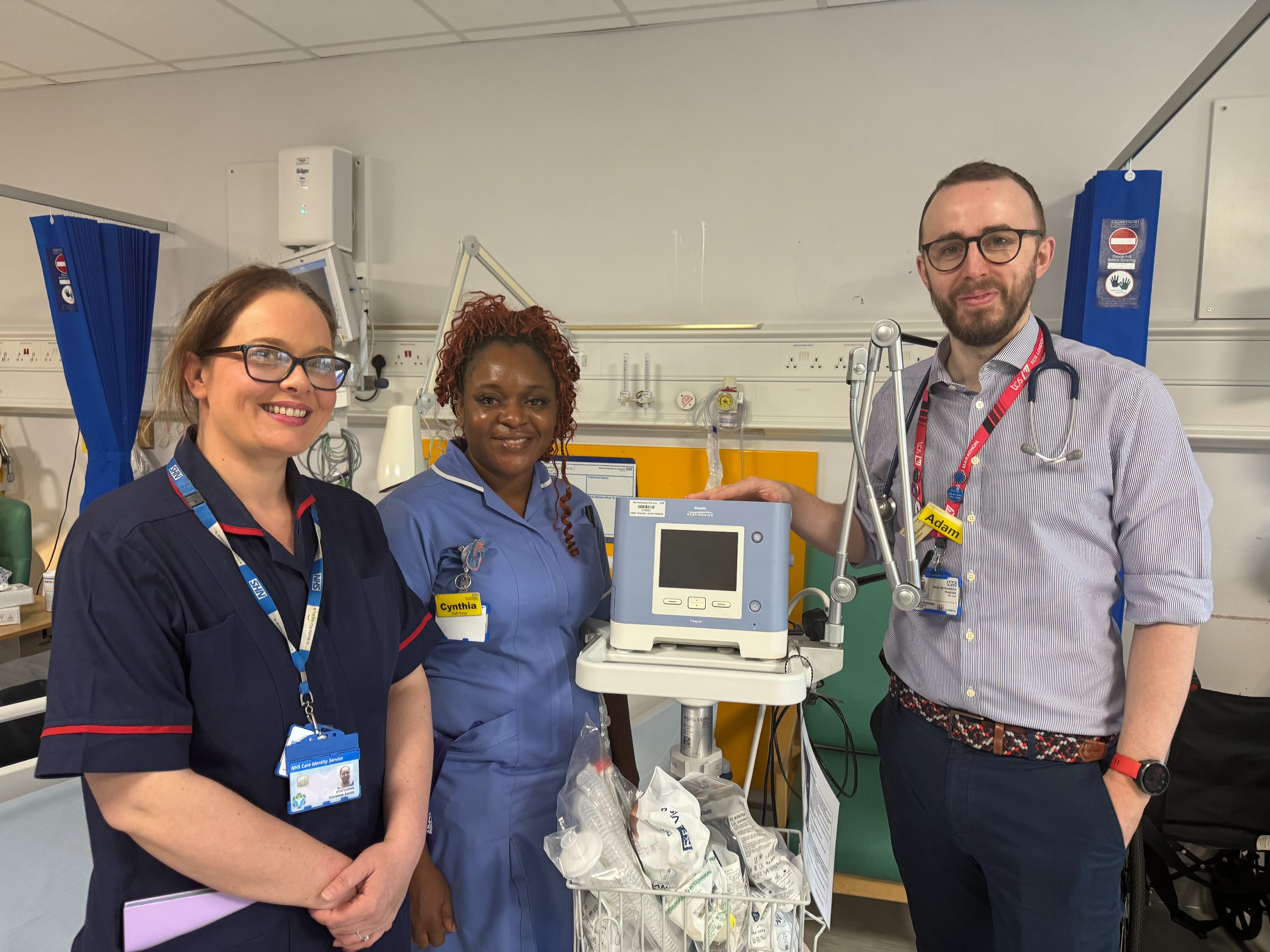
Hospital project results in thousands of pressure ulcer-free days for patients
Date published: 4 July 2025
-

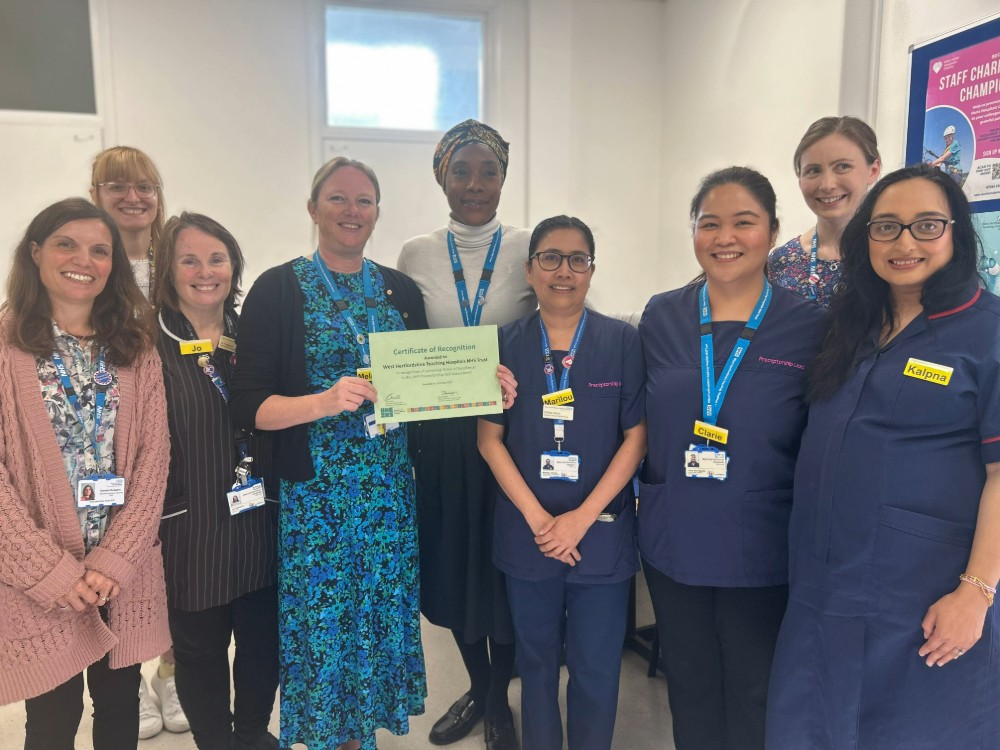
Excellence awards for ‘exceptional colleagues’ putting babies and families at the heart of care
Date published: 24 June 2025
-

Most in-depth evaluation of Hospital at Home to date reveals millions in savings, better outcomes and sky-high patient satisfaction
Date published: 13 June 2025
-
Specialist nurse ‘treated like royalty’ at Buckingham Palace garden party
Date published: 11 June 2025
-
Top marks for programme helping newly qualified NHS staff
Date published: 9 June 2025
-

Volunteers with a 'lot of heart’ needed at Watford General Emergency Department
Date published: 3 June 2025
-

Local service at Hemel Hospital celebrates 20 years of excellence
Date published: 29 May 2025
-

Hemel Hempstead Health Campus programme director takes up role
Date published: 14 May 2025
-

Redevelopment of Watford General Hospital takes step forward with £12m funding for next phase of the scheme
Date published: 8 May 2025