-

Confirmed industrial action by resident doctors 17-22 December
Date published: 10 December 2025
-

West Herts named NHS Trust of the Year
Date published: 21 November 2025
-

West Herts Launches New Clinical Strategy to Shape the Future of Care
Date published: 18 November 2025
-

Confirmed industrial action by resident doctors: 14-19 November
Date published: 10 November 2025
-
'Extraordinary’ emergency staff at Watford General recognised during first ‘A&E Appreciation Week’
Date published: 15 October 2025
-
New staff wellbeing room opens at St Albans City Hospital following successful community fundraising
Date published: 18 September 2025
-
First-of-its-Kind Partnership to Revolutionise Community Healthcare in the UK
Date published: 11 September 2025
-

West Herts nominated for NHS Trust of the Year in national awards
Date published: 11 August 2025
-
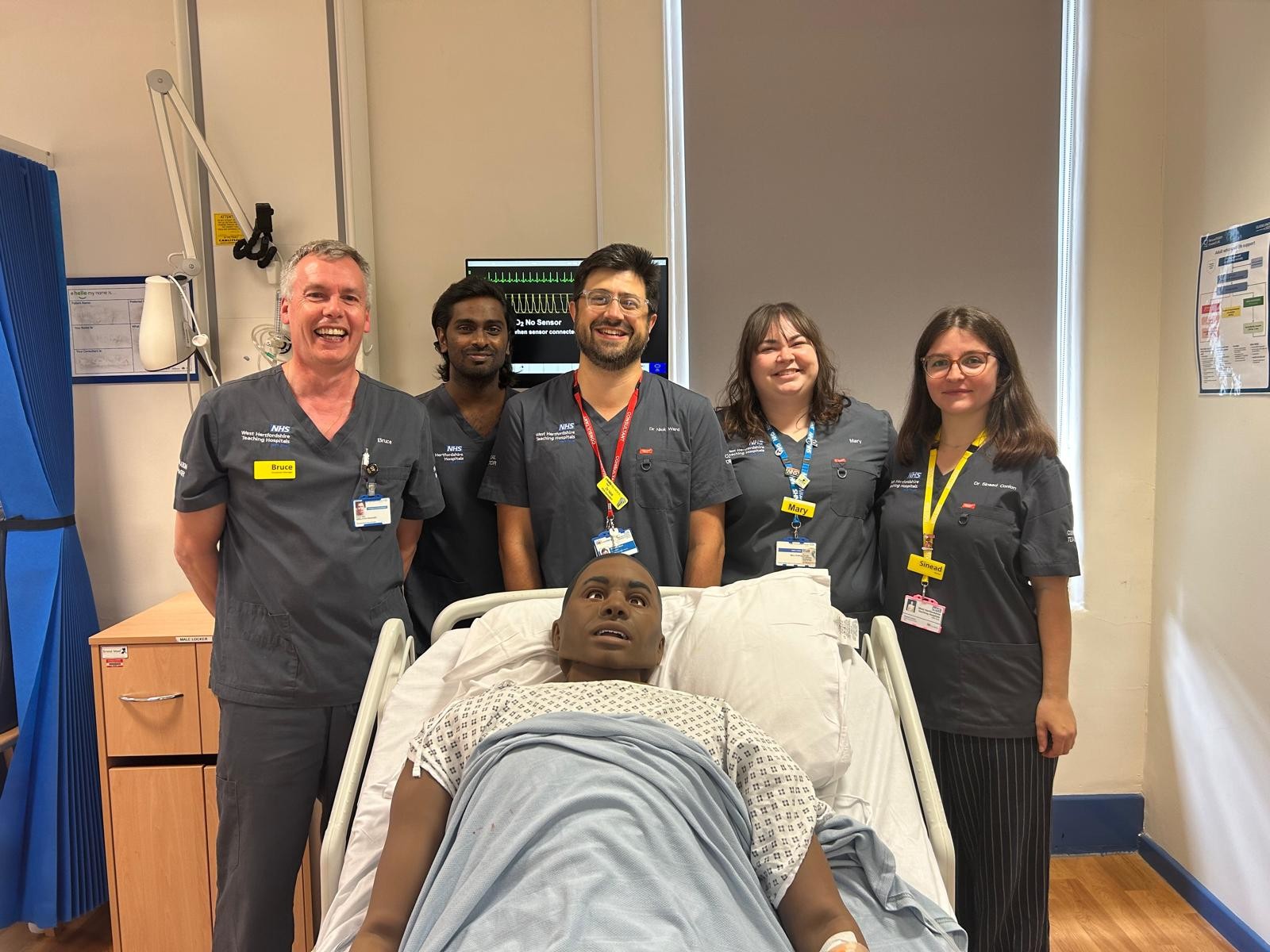
Simulation education team is nationally accredited as centre for excellence
Date published: 7 August 2025